The overwhelming majority of health professionals and researchers, including doctors, nurses, and psychologists who were interviewed through a survey agree that there should be ethical criteria for the admission of patients with COVID-19 to intensive care units, in the event of a situation of scarcity of material and/or human resources.
This is one of the preliminary results of a survey carried out at the Faculty of Medicine of the University of Porto (FMUP) and at CINTESIS – Center for Health Technology and Services Research, and which will be extended to all national medical schools in the coming days.
 The study is coordinated by Rui Nunes (professor at FMUP and specialist in Bioethics) and Altamiro Costa-Pereira (director of FMUP), and is assisted by Olga Magalhães (FMUP / CINTESIS). It was carried out in record time and the aim is to answer a number of questions that have already been asked in other countries, such as Spain and Italy, in view of the disproportion of seriously and very seriously ill COVID-19 patients needing intensive care in view of the means available to treat them.
The study is coordinated by Rui Nunes (professor at FMUP and specialist in Bioethics) and Altamiro Costa-Pereira (director of FMUP), and is assisted by Olga Magalhães (FMUP / CINTESIS). It was carried out in record time and the aim is to answer a number of questions that have already been asked in other countries, such as Spain and Italy, in view of the disproportion of seriously and very seriously ill COVID-19 patients needing intensive care in view of the means available to treat them.
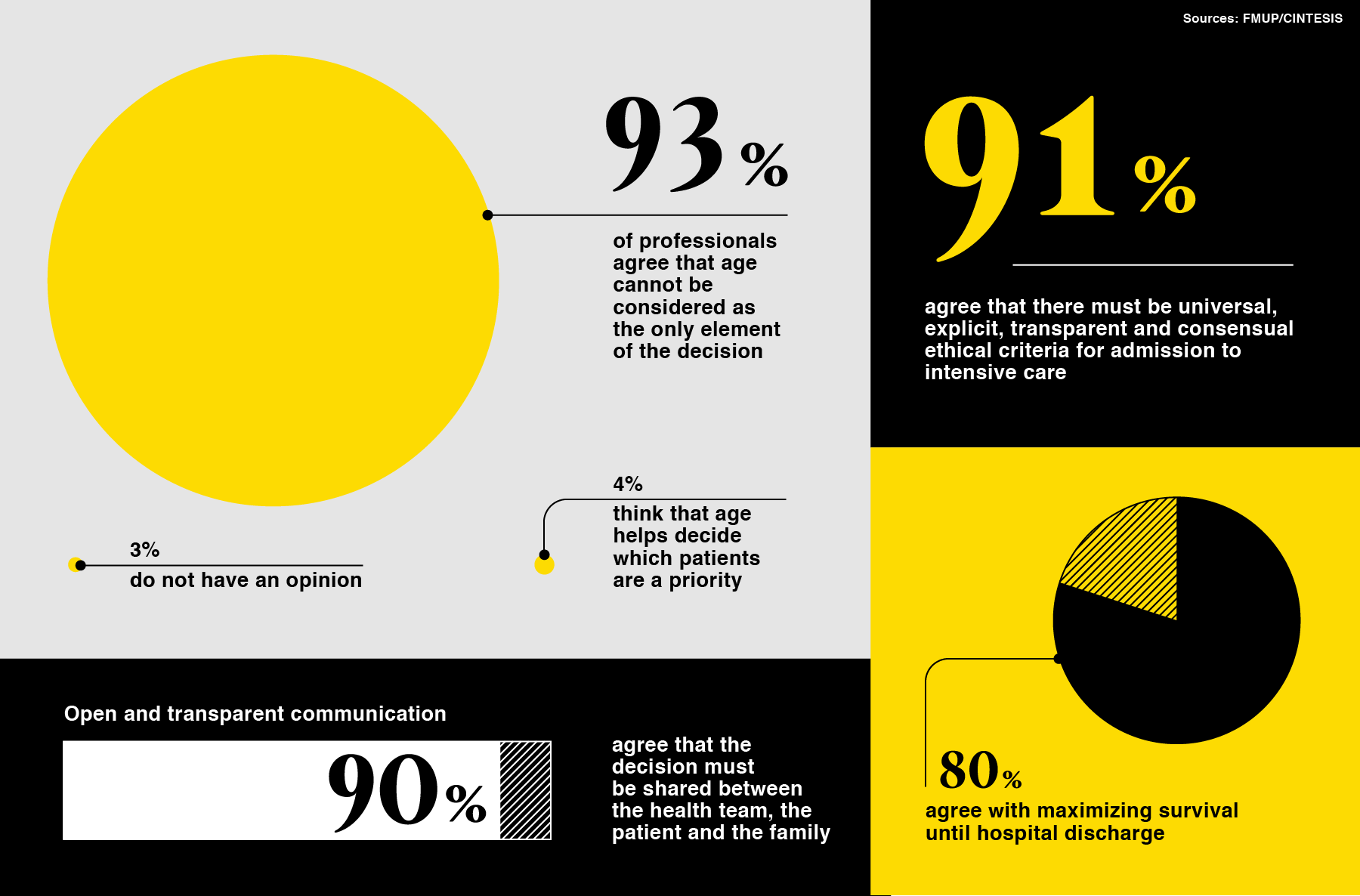
Of the more than 350 health professionals and researchers who responded to the online survey, 91% consider that, in addition to clinical criteria, there must be “universal, explicit, transparent and consensual ethical criteria for admission to intensive care”. Only 6% do not see the need for such ethical criteria and 3% have no opinion on the topic.
Almost 90% of respondents also agree that the decision must be shared between the health team, the patient and the family, in order to promote “open and transparent communication”. Only 8% say they don’t agree with such a shared decision and 3% don’t have an opinion.
As for the criteria that should preside over the decision to admit a certain patient with COVID-19 in detriment to another, the vast majority believes that age should not be decisive. After all, 93% of professionals agree that age cannot be considered as the only element of the decision. Only 4% of respondents think that age serves to decide which patients are a priority, and 3% confess to not having an opinion.
About 80% of professionals understand that, given the impossibility of admitting all patients with COVID-19 at the same time, “maximizing survival until hospital discharge” must be valued. The same is to say that most professionals admit that, if it is necessary to choose, priority should be given to patients who are more likely to survive. Only 7% disagree and 13% have no opinion.
The consensus is not so great with respect to another possible criterion in prioritizing patients to be admitted to intensive care: the number of years saved. About 66% of professionals believe that “maximizing the number of years of life saved” should be valued, while 18% say they do not agree with that criterion and 16% admit they do not have an opinion.
Opinions are even more divided with regard to the application of the so-called “opportunity cost principle”, avoiding as an absolute rule the criterion “first to arrive first to admit”. In all, 56% of respondents answered yes, that the “opportunity cost” must be taken into account, which implies that admission must not always be made on a first-come, first-served basis. However, 27% disagree and 17% have no opinion.
This survey was carried out from April 6 to 11. 51% of respondents are doctors and 73% of those are under 50 years of age.

